Abstract:Phimosis and paraphimosis are two significant urological conditions affecting the foreskin of the penis. This article explores their etiology, pathophysiology, clinical manifestations, diagnostic approaches, and management strategies, providing a comprehensive overview for healthcare professionals.Introduction:Phimosis and paraphimosis represent distinct pathological states of the penile foreskin, each with unique clinical implications. Phimosis is characterized by the inability to retract the foreskin over the glans penis, while paraphimosis involves the entrapment of the retracted foreskin behind the glans, leading to potential complications.Etiology and Pathophysiology:Phimosis can be classified as either physiological or pathological. Physiological phimosis is common in neonates and young children and typically resolves spontaneously with age. Pathological phimosis, however, may arise from repeated infections, inflammation, or trauma leading to scarring and fibrosis of the foreskin. Common etiological factors include balanitis, lichen sclerosus, and poor hygiene.Paraphimosis occurs when the foreskin is retracted behind the glans penis and cannot be returned to its normal position. This condition is often iatrogenic, resulting from improper retraction during catheterization or physical examination. The constricted foreskin impairs venous and lymphatic drainage, leading to edema and, potentially, ischemia of the glans.Clinical Manifestations:Phimosis is often asymptomatic but may present with difficulties in urination, recurrent infections, or painful erections. In severe cases, the patient may experience a ballooning of the foreskin during micturition or paraphimosis as a complication.Paraphimosis is typically an acute condition and presents with pain, swelling, and erythema of the glans penis. The constriction may cause significant discomfort and, if untreated, can progress to tissue necrosis due to compromised …

Phimosis and Paraphimosis: Clinical Perspectives and Management Approaches
Abstract:
Phimosis and paraphimosis are two significant urological conditions affecting the foreskin of the penis. This article explores their etiology, pathophysiology, clinical manifestations, diagnostic approaches, and management strategies, providing a comprehensive overview for healthcare professionals.
Introduction:
Phimosis and paraphimosis represent distinct pathological states of the penile foreskin, each with unique clinical implications. Phimosis is characterized by the inability to retract the foreskin over the glans penis, while paraphimosis involves the entrapment of the retracted foreskin behind the glans, leading to potential complications.
Etiology and Pathophysiology:
Phimosis can be classified as either physiological or pathological. Physiological phimosis is common in neonates and young children and typically resolves spontaneously with age. Pathological phimosis, however, may arise from repeated infections, inflammation, or trauma leading to scarring and fibrosis of the foreskin. Common etiological factors include balanitis, lichen sclerosus, and poor hygiene.
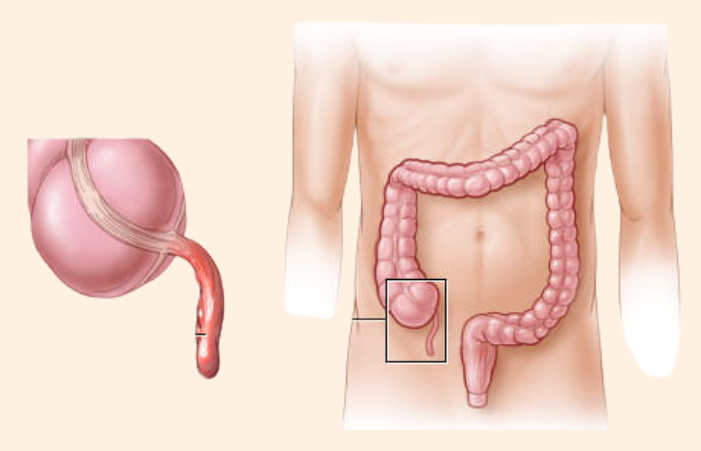
Paraphimosis occurs when the foreskin is retracted behind the glans penis and cannot be returned to its normal position. This condition is often iatrogenic, resulting from improper retraction during catheterization or physical examination. The constricted foreskin impairs venous and lymphatic drainage, leading to edema and, potentially, ischemia of the glans.
Clinical Manifestations:
Phimosis is often asymptomatic but may present with difficulties in urination, recurrent infections, or painful erections. In severe cases, the patient may experience a ballooning of the foreskin during micturition or paraphimosis as a complication.
Paraphimosis is typically an acute condition and presents with pain, swelling, and erythema of the glans penis. The constriction may cause significant discomfort and, if untreated, can progress to tissue necrosis due to compromised blood flow.
Diagnosis:
The diagnosis of phimosis is primarily clinical and involves a detailed history and physical examination. The key feature is the inability to retract the foreskin, and secondary findings may include signs of infection or inflammation. Diagnostic imaging is rarely required unless there is suspicion of underlying anatomical anomalies.
Paraphimosis is diagnosed through physical examination, which reveals the retracted foreskin and engorged glans. The constricted foreskin is often visible as a tight band around the penis. Rapid assessment is crucial to prevent ischemic complications.
Management Strategies:
The management of phimosis depends on the severity and underlying cause. Conservative treatments include topical corticosteroids, which can reduce inflammation and facilitate foreskin retraction. Gentle, gradual stretching exercises may also be beneficial. In cases where conservative measures fail, circumcision or preputioplasty may be indicated to relieve symptoms and prevent complications.
Paraphimosis is a medical emergency requiring prompt intervention to prevent ischemic damage. Initial management involves manual reduction, where gentle compression of the glans is applied to reduce edema, followed by repositioning of the foreskin. If manual reduction is unsuccessful, a dorsal slit or circumcision may be required to alleviate the constriction. Analgesics and anti-inflammatory medications are often administered to manage pain and swelling.
Prevention and Long-term Care:
Preventing phimosis involves maintaining proper genital hygiene and addressing any underlying infections or inflammatory conditions. Parents should be educated about the natural development of the foreskin and the importance of not forcefully retracting it in young children.
Preventing paraphimosis primarily involves ensuring proper handling of the foreskin during medical procedures. Healthcare providers should be trained to retract and replace the foreskin correctly to avoid iatrogenic injury. Patients and caregivers should be instructed on the proper care of the foreskin, especially after catheterization or other urological interventions.
Complications:
Complications of untreated phimosis include recurrent infections, obstructive uropathy, and an increased risk of penile carcinoma due to chronic inflammation. Severe phimosis can also lead to paraphimosis, causing further complications.
Paraphimosis, if not promptly treated, can result in glans ischemia, necrosis, and eventual penile amputation in extreme cases. Chronic paraphimosis may predispose to recurrent episodes and scarring, necessitating surgical intervention.
Conclusion:
Phimosis and paraphimosis are important clinical conditions that require appropriate recognition and management to prevent serious complications. Understanding the pathophysiology, clinical presentation, and treatment options is essential for effective management and prevention. Comprehensive patient education and healthcare provider training are key to reducing the incidence and impact of these conditions.
Future Directions:
Research into non-surgical interventions and novel therapeutic agents for phimosis is ongoing and may offer improved outcomes for patients. Advances in surgical techniques and post-operative care continue to enhance the management of paraphimosis, reducing morbidity and improving patient quality of life.
References:
Chart: Differences Between Phimosis and Paraphimosis
Characteristic | Phimosis | Paraphimosis |
Definition | Inability to retract the foreskin over the glans penis. | Foreskin retracted behind the glans and cannot return to its original position. |
Primary Cause | Developmental or pathological changes like scarring or inflammation. | Often iatrogenic or due to trauma, improper handling, or infection. |
Age of Onset | Common in infants and young children; can occur in adults due to pathological reasons. | Can occur at any age, often related to medical procedures or injury. |
Symptoms | Difficulty urinating, ballooning of foreskin, painful erections, recurrent infections. | Pain, swelling, erythema of the glans, potential ischemia and necrosis. |
Common Complications | Recurrent infections, obstructive uropathy, increased risk of penile carcinoma. | Glans ischemia, necrosis, potential penile amputation if untreated. |
Diagnosis | Clinical examination showing non-retractable foreskin, possible signs of infection or scarring. | Clinical examination revealing retracted foreskin trapped behind glans. |
Initial Management | Topical corticosteroids, gentle foreskin stretching exercises, maintaining hygiene. | Manual reduction of the foreskin, application of cold packs to reduce swelling. |
Surgical Intervention | Circumcision or preputioplasty in severe or non-responsive cases. | Emergency dorsal slit or circumcision if manual reduction fails. |
Prevention | Proper hygiene, avoiding forceful retraction, treating underlying infections. | Proper handling during medical procedures, education on foreskin care. |
Pain | Usually mild or absent unless complicated by infection or severe phimosis. | Typically severe and acute, requiring immediate medical attention. |
Prognosis | Generally good with appropriate treatment, most cases resolve without surgery. | Good if treated promptly; risk of complications increases with delayed treatment. |
Recurrence Risk | Low after treatment, higher if underlying causes like chronic inflammation persist. | Potential for recurrence if foreskin is improperly handled again. |
Imaging Required | Rarely needed, unless anatomical anomalies are suspected. | Not typically required unless assessing for complications. |
Underlying Conditions | Can be associated with conditions like lichen sclerosus or diabetes. | Often related to improper foreskin handling or trauma. |
Patient Education | Educate on natural development of foreskin, importance of gentle handling. | Emphasize the importance of repositioning the foreskin after retraction. |
Emergency Status | Not an emergency unless leading to severe complications. | Considered a urological emergency requiring immediate intervention. |
Long-term Management | Regular monitoring, ensuring no recurrence of infections or inflammation. | Monitoring for signs of ischemia or complications post-treatment. |
Prognostic Indicators | Dependent on cause; better prognosis with early treatment of underlying conditions. | Prognosis depends on timeliness of intervention and absence of complications. |
Incidence | Common in neonates; less common in adults unless due to specific conditions. | Less common, often related to specific incidents like catheterization. |
Treatment Duration | May require weeks of topical treatment; surgical recovery if needed. | Immediate intervention required; recovery depends on extent of initial damage. |
Impact on Urination | May cause obstructive symptoms or difficulty with urination. | Typically causes acute pain and swelling, which may impair urination. |
Role of Hygiene | Critical in preventing infections that can lead to or exacerbate phimosis. | Important for preventing infections that may lead to complications. |
This chart outlines the key differences between phimosis and paraphimosis, focusing on their definitions, causes, symptoms, management, and prevention. Proper understanding of these distinctions is crucial for effective diagnosis and treatment.
Chart: Differences Between Conventional Circumcision and ZSR Stapler Surgery
Characteristic | Conventional Circumcision | ZSR Stapler Surgery |
Definition | Surgical removal of the foreskin using a scalpel or scissors. | A device-based circumcision method using a stapler to excise the foreskin and simultaneously staple the wound. |
Procedure Duration | Typically takes 20-30 minutes. | Generally completed in 5-10 minutes. |
Surgical Technique | Manual excision of the foreskin followed by suturing. | The foreskin is clamped, cut, and stapled using a single device. |
Anesthesia | Local or general anesthesia, depending on age and patient preference. | Local anesthesia; less invasive and quicker. |
Bleeding Control | Achieved through careful surgical technique and suturing. | Minimal bleeding due to simultaneous cutting and stapling. |
Postoperative Pain | Moderate pain managed with analgesics. | Typically less pain due to minimal tissue handling and quicker procedure. |
Wound Closure | Closed with sutures or surgical glue. | Closed with staplers that remain in place until healing. |
Healing Time | Approximately 2-4 weeks for complete healing. | Faster healing, generally within 1-2 weeks. |
Scarring | Varies depending on technique and healing; potential for visible scars. | Minimal and more uniform scarring due to precise cutting and stapling. |
Infection Risk | Moderate, depending on post-op care and technique. | Lower infection risk due to quicker procedure and minimal handling. |
Complication Rates | Higher risk of complications like excessive bleeding, infection, or scarring. | Lower complication rates due to minimal tissue trauma and quick procedure. |
Aesthetic Outcome | Dependent on surgeon’s skill; potential for varied cosmetic results. | Generally more consistent and aesthetically pleasing outcomes. |
Suture Removal | Required 7-10 days post-surgery. | No suture removal needed; staples fall off naturally. |
Patient Age Suitability | Suitable for all ages, from infants to adults. | Primarily recommended for older children and adults due to device size. |
Postoperative Care | Regular wound cleaning, monitoring for infection, pain management. | Minimal care; usually involves regular cleaning and monitoring for staple loss. |
Recovery Time | Longer recovery due to suture healing process. | Shorter recovery time due to rapid wound closure and minimal intervention. |
Rehabilitation | Avoid strenuous activity for 4-6 weeks. | Normal activity can often resume within a week. |
Cosmetic Control | Surgeon has more control over the final appearance. | Device determines the final appearance, which is usually consistent. |
Technique Variability | Various techniques and modifications available. | Standardized technique with minimal variability. |
Cost | Varies widely; generally lower compared to ZSR stapler. | Usually higher due to the cost of the stapler device. |
Availability | Widely available globally. | Limited to facilities with access to the ZSR device. |
Training Requirement | Requires extensive surgical training and experience. | Requires specific training on the ZSR stapler device. |
Postoperative Sensation | Risk of altered sensation due to extensive tissue removal. | Typically less impact on sensation due to precision cutting. |
Tissue Handling | Manual tissue handling can increase risk of trauma and scarring. | Minimal tissue handling reduces trauma and scarring. |
Patient Comfort | Less comfortable due to longer procedure and suture irritation. | More comfortable due to quick procedure and no suture irritation. |
Accessibility | Widely accessible in most healthcare settings. | Limited to specialized centers with the device. |
Surgeon Dependency | Highly dependent on the surgeon’s skill and technique. | Less dependent on skill; device ensures consistent results. |
Complication Management | Requires close monitoring for bleeding and infection. | Minimal complications; easier to manage if they arise. |
Ideal Candidates | Suitable for all patients needing foreskin removal. | Ideal for patients seeking quick recovery and minimal pain. |
Cultural Acceptance | Widely accepted in various cultural and religious contexts. | Less known and accepted in some cultural settings. |
Long-term Outcomes | Effective with a range of long-term results based on technique. | Effective with consistent long-term results. |
Reversible Option | Irreversible; once performed, foreskin cannot be restored. | Irreversible; foreskin cannot be reattached or restored. |
Medical Device Requirement | No specific device required, just standard surgical tools. | Requires a specialized ZSR stapler device. |
Technical Complexity | Higher complexity due to manual technique and suturing. | Lower complexity; device simplifies the procedure. |
Potential for Misuse | Higher risk if performed by untrained individuals. | Lower risk due to standardized device usage. |
This chart highlights the differences between conventional circumcision and ZSR stapler surgery, focusing on aspects such as procedure, healing, patient outcomes, and accessibility. Understanding these differences can help in making informed decisions regarding circumcision methods.